Traditional healthcare boundaries blur as payers, retailers, and providers converge.

The healthcare industry is witnessing a significant transformation marked by the blurring of traditional boundaries among key players like health systems, insurers, retailers, and tech firms. Major industry giants such as CVS Health, Amazon, and Walgreens are driving this shift by aggressively expanding their presence in healthcare. Simultaneously, hospitals are adopting consumer-centric strategies from the retail sector, focusing on convenience, accessibility, and personalized patient experiences.
According to the Philips Future Health Index 2021 Report, healthcare leaders across 14 countries anticipate a substantial change in care delivery, with 23% of care visits projected to take place outside traditional hospital settings. This highlights the increasing importance of alternative care models prioritizing patient convenience and accessibility.
A notable trend in this transformation is the emergence of hybrid designations like “payvider,” signifying collaborative partnerships between payers and providers. These alliances aim to mitigate financial risks, boost profitability, enhance the patient experience, and ultimately achieve better health outcomes. Examples include joint ventures between healthcare entities such as Banner Health and Aetna, Aurora, and Anthem, as well as initiatives like Humana offering insurance alongside healthcare provision.
This convergence of healthcare stakeholders reflects a fundamental shift towards more patient-centric, accessible, and convenient healthcare delivery models. By breaking down traditional industry silos and fostering collaboration, stakeholders are striving to create a healthcare ecosystem that better meets patient needs, driving improved outcomes and experiences.
Evolving Roles
Retailers, providers, and payers are experiencing more flexible roles and fluid boundaries in their responsibilities. Payers, traditionally focused on financing healthcare, are now adopting consumer-centric approaches. For instance, Humana’s expansion of CenterWell primary care centers showcases a shift towards vertical integration in the payer sector, emphasizing collaboration with providers. Retailers like CVS, Kroger, Costco, Amazon, and Walmart are meeting the demand for accessible healthcare services. Initiatives such as Kroger’s transition of in-store clinics into primary care centers and Costco’s partnership with Sesame for discounted outpatient services highlight their efforts to expand in healthcare. Meanwhile, healthcare providers are embracing consumer-centric principles to meet patient expectations. Collaborations with retailers and tech firms, like Pearl Health and Walgreens, aim to enhance accessibility. Partnerships between health systems and Amazon’s One Medical prioritize preventive services through value-based care models.
Convergence and Partnerships
So how is the the convergence of payers, retailers, and providers reshaping the healthcare landscape? Driven by a shared goal of delivering value-based, patient-centric care, these collaborative efforts signify a strategic realignment towards integrated care delivery. Experts expect these partnerships to mprove access, reduce costs, and enhance patient experiences through coordinated care delivery.
Here are some additional benefits of partnerships between healthcare entities:
- Enhanced access to care: By combining resources and services, converged entities can create more accessible healthcare delivery models. This includes placing clinics in retail locations, offering telehealth services, and extending hours of operation, providing patients with greater flexibility in accessing care.
- Improved coordination of care: Converged entities can streamline communication and information sharing between payers, retailers, and providers, leading to better coordination and continuity of care. This can reduce medical errors, duplication of services, and gaps in care, resulting in improved health outcomes for patients.
- Cost savings: By integrating services and resources, converged entities can achieve economies of scale and operational efficiencies, leading to cost savings. This can result in lower healthcare costs for both patients and payers, making healthcare more affordable and accessible to a broader population.
- Patient-centric approach: Convergence enables a more patient-centric approach to healthcare delivery, focusing on meeting the individual needs and preferences of patients. This can include personalized care plans, tailored wellness programs, and enhanced patient engagement, resulting in higher patient satisfaction and improved health outcomes.
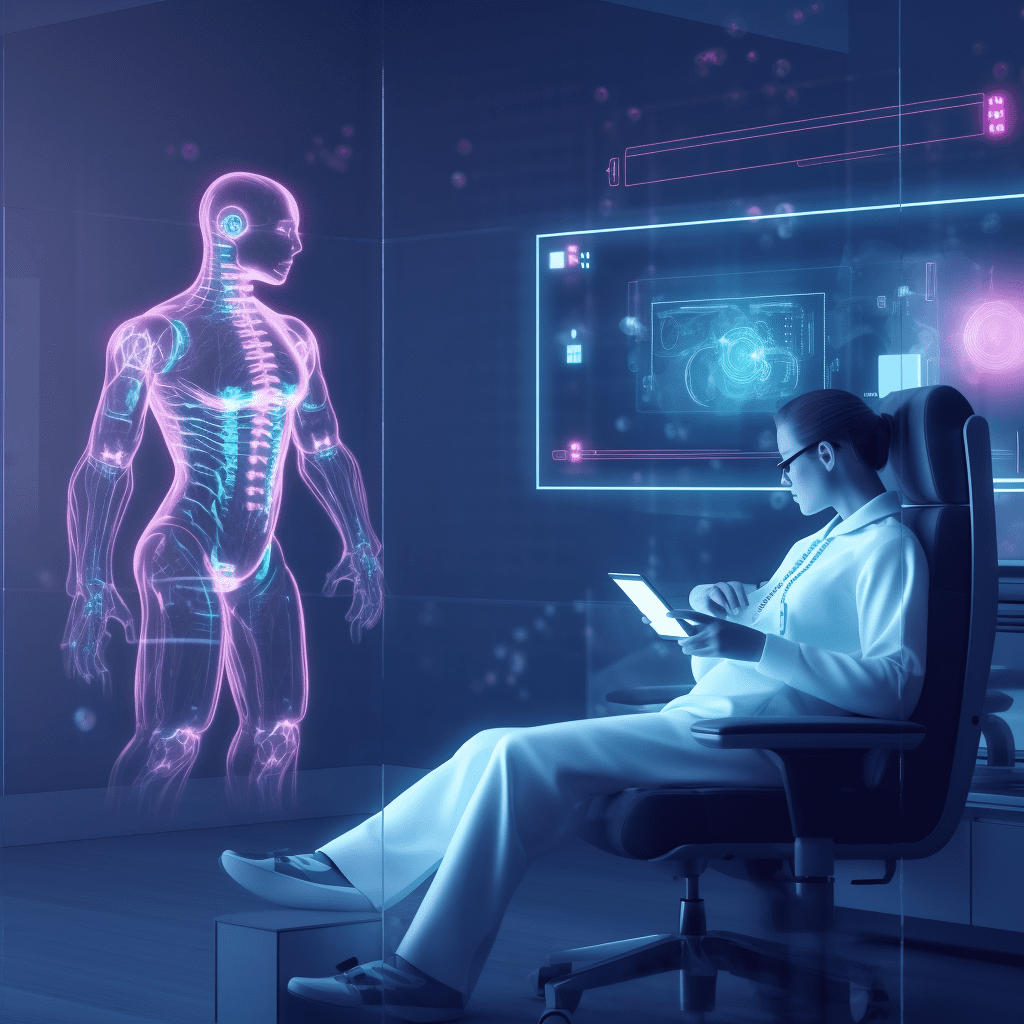
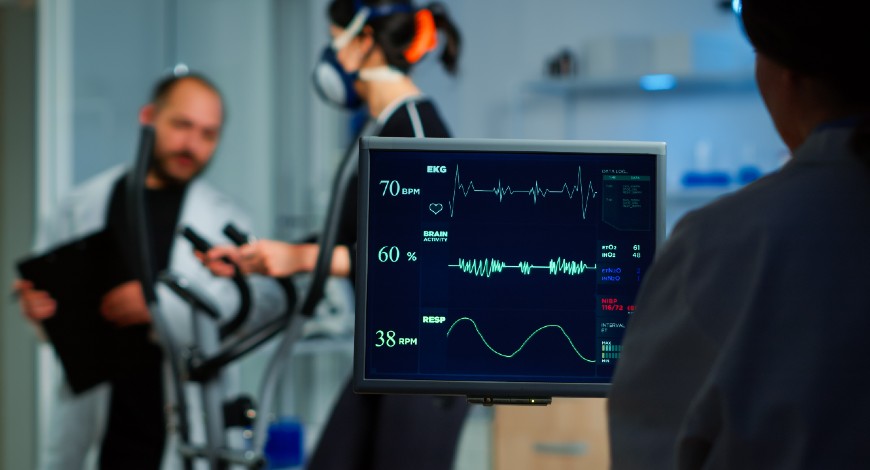
- Innovation and technological advancements: Converged entities have the resources and expertise to invest in innovative technologies and solutions to improve healthcare delivery. This can include digital health platforms, remote monitoring devices, and artificial intelligence tools, enhancing the quality and efficiency of care delivery.
- Expanded scope of services: By bringing together payers, retailers, and providers, converged entities can offer a broader range of services to patients. This can include preventive care, chronic disease management, behavioral health services, and social determinants of health support, addressing the comprehensive needs of patients.
- Community health improvement: Converged entities are well-positioned to address the social determinants of health and promote community health improvement initiatives. This can include partnerships with community organizations, investment in public health programs, and initiatives to address healthcare disparities, leading to healthier communities overall.