Integrating data to enable clinical collaboration and patient-centered care

Multidisciplinary care teams are finding it more difficult than ever to stay in touch with one another and to stay on top of all the pertinent information about their patients, including demographic information, medical histories, and a range of subspecialty reports. Selecting the appropriate treatment is equally difficult, particularly in fields like oncology where patients and doctors may be faced with an overwhelming array of options.
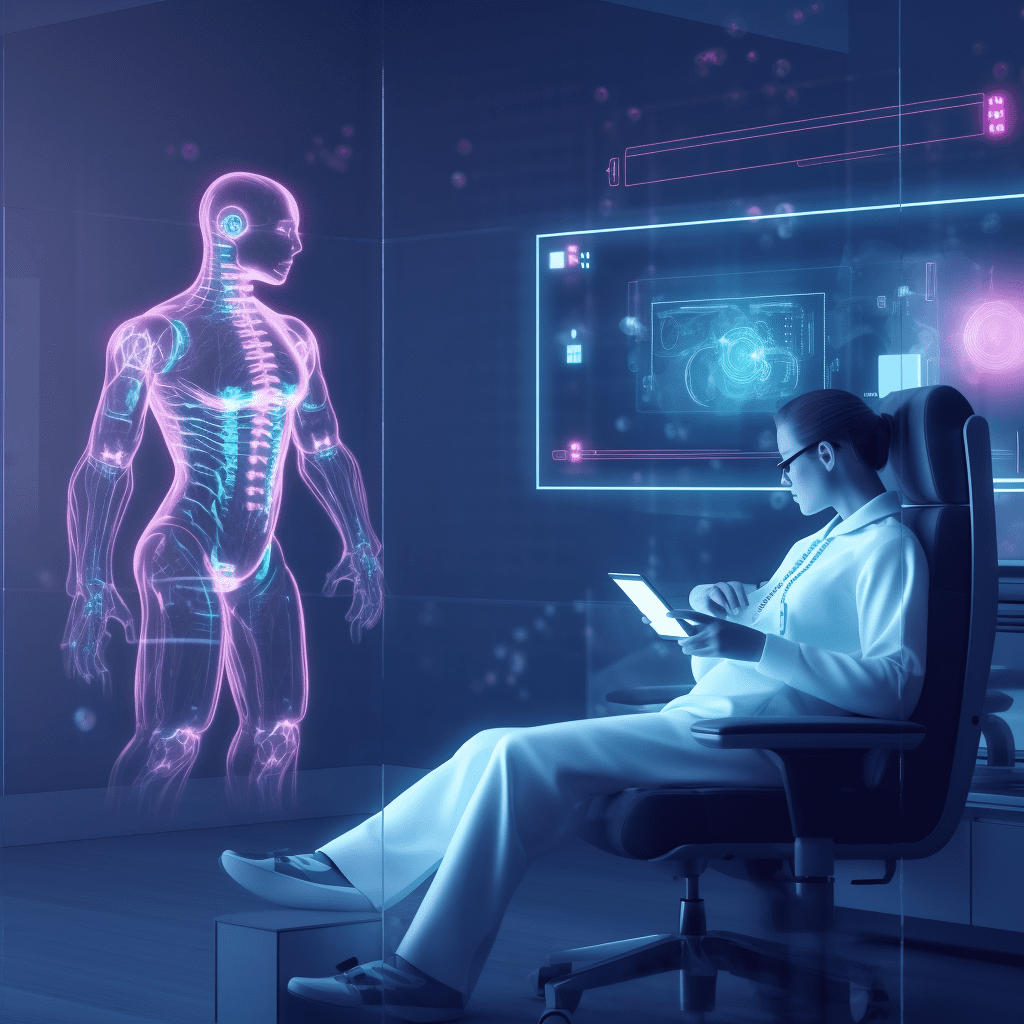
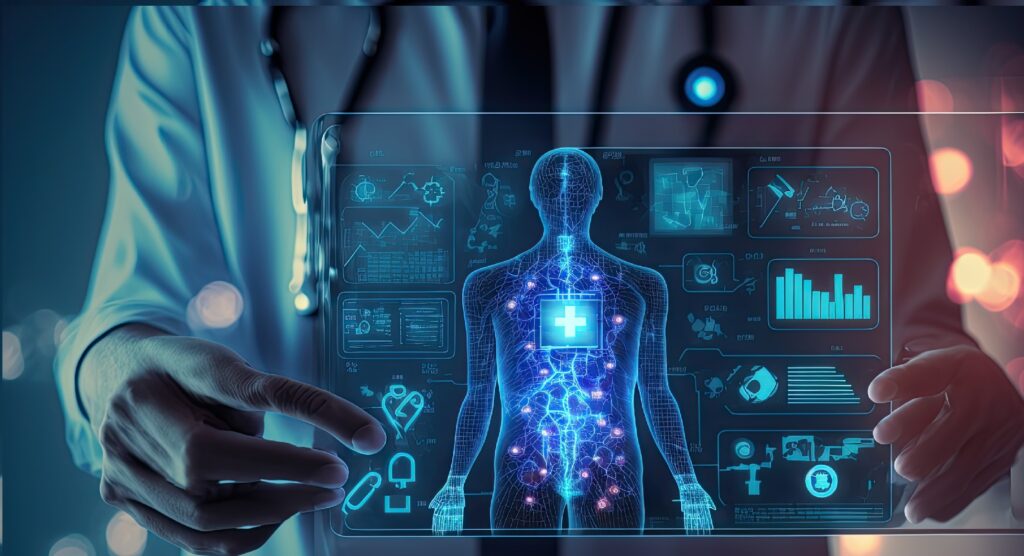
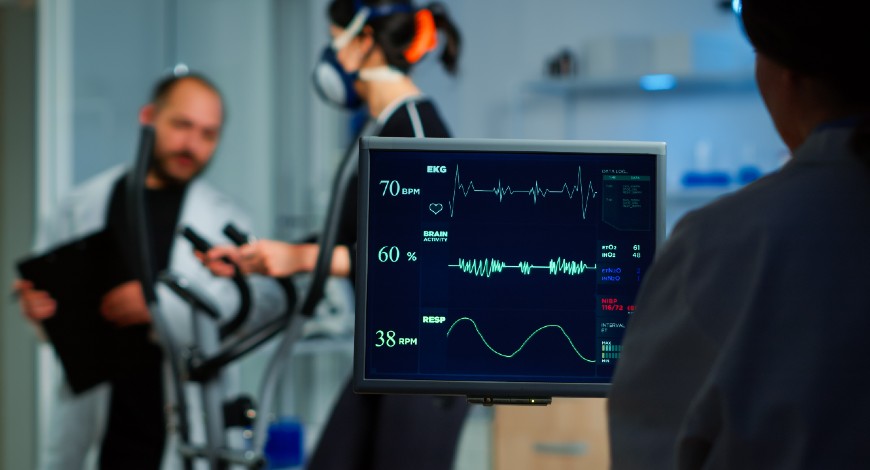
Integrated diagnostics is a quickly developing sector in which companies utilize intelligent, networked systems to combine imaging, monitoring, laboratory, genomics, and longitudinal data to provide them with complete and useful insights into their patient populations. An excellent illustration of this development in healthcare technology is multidisciplinary tumor boards. Care teams may now provide comprehensive, patient-centered cancer care thanks to integrated diagnostics systems. By combining patient data from many sources into dashboards, these solutions enable collaborative decisions about diagnosis, treatment, and follow-up.
However, this does not imply that oncology decision-making will ever be entirely automated. As a matter of fact, the objective of this trend in healthcare technology is not so much to replace human labor with automation as it is to provide care teams with pertinent, evidence-based guidance to facilitate joint decision-making with patients, ensuring that the latter make the decisions that will enable them to live as long and as well as possible.
The similar strategy is being used in cardiology, where integrated diagnostics systems that are improved by predictive analytics and intelligent algorithms enable cardiology care teams to make clinical choices more quickly by providing pertinent and useful information that enhances patient care.